Introduction
Fibrinogen is a vital protein in the blood that plays a central role in hemostasis—the process that stops bleeding by forming clots. As a precursor to fibrin, it not only helps create blood clots but also contributes to immune responses, inflammation, and chronic disease processes. Measuring fibrinogen levels is a key diagnostic tool for evaluating conditions like excessive bleeding, disseminated intravascular coagulation (DIC), and for monitoring liver or inflammatory diseases.
🔹 Understanding Fibrinogen: Its Role and Importance
✅ Molecular Structure
Fibrinogen is a glycoprotein found in blood plasma, produced by liver cells. It consists of three polypeptide chains (Aα, Bβ, and γ), linked together by disulfide bonds. With a molecular weight of about 340 kDa, it’s a complex protein essential to bodily functions.
✅ Biological Functions
Fibrinogen serves several critical purposes in the body:
- Conversion to Fibrin: When bleeding occurs, the enzyme thrombin transforms fibrinogen into fibrin. Fibrin forms a web-like structure that traps blood cells to create a clot, effectively halting blood loss.
- Binding to Platelet Receptors: Fibrinogen attaches to GPIIb/IIIa receptors on platelets, helping them stick together and adhere to injured tissue. This step is crucial for clot formation.
- Acute Phase Response: As an acute phase reactant, fibrinogen levels rise during inflammation, aiding the body’s response to infections or injuries.
- Wound Healing: Fibrinogen supports tissue repair by forming a scaffold that encourages new cell growth at wound sites.
🔹 Clinical Uses of the Fibrinogen Test
- Diagnosing and Monitoring DIC (Disseminated Intravascular Coagulation)
DIC is a serious condition where clotting and clot breakdown occur abnormally throughout the body. Fibrinogen levels are a key marker for diagnosing and tracking DIC, as low levels may indicate excessive consumption during widespread clotting. - Investigating Unexplained Bleeding
Abnormal fibrinogen levels can help pinpoint the cause of mysterious bleeding. A drop in fibrinogen might suggest clotting disorders, such as liver issues or DIC, that lead to excessive bleeding. - Assessing Advanced Liver Disorders
Since the liver produces fibrinogen, advanced liver conditions like cirrhosis can reduce its levels. Testing fibrinogen helps gauge liver function and diagnose related problems. - Monitoring Primary or Secondary Fibrinolysis
Fibrinolysis is the process of breaking down clots. Low fibrinogen levels can signal excessive fibrinolysis, making the test valuable for tracking this condition and related issues. - Measuring Acute Phase Response in Inflammation or Cancer
Fibrinogen rises during inflammation or malignancy as an acute phase protein. Testing its levels can assess the severity of inflammation or monitor cancer progression. - Predicting Cardiovascular Disease Risk
Elevated fibrinogen is a known risk factor for heart and vascular diseases. High levels can increase the likelihood of clot formation, potentially leading to blockages, heart attacks, or strokes.
🔹 Laboratory Methods for Measuring Fibrinogen
- Clauss Method (Reference Standard)
- How It Works: High-concentration thrombin is added to plasma, and the time it takes to clot is measured. This is the gold standard for assessing fibrinogen activity.
- Reporting Units: Results are given in milligrams per deciliter (mg/dL) or grams per liter (g/L).
Today, most commercial kits use this method to measure fibrinogen. The Heamostica Fibrinogen kit also uses the Clauss method. To view the brochure and production license for the Heamostica Fibrinogen kit, please refer to the following link:
Heamostica Fibrinogen Kit
- Immunologic Method (Nephelometry/ELISA)
- How It Works: This method measures fibrinogen antigen levels (not its activity) by focusing on the protein’s presence in plasma.
- Use: It’s helpful for distinguishing between dysfibrinogenemia (structural defects) and hypofibrinogenemia (low levels), as it reveals whether the issue lies in function or quantity.
- Viscoelastic Methods (ROTEM/TEG)
- Use: Commonly used during surgery, trauma, or acute bleeding, these tests evaluate clot dynamics in real time.
- Benefit: They’re especially useful in emergencies like trauma or major surgery, providing ongoing insights into clotting behavior.
🔹 Clauss Method in Detail
The Clauss method hinges on the principle that clotting time in diluted plasma, when mixed with high-concentration thrombin, directly correlates with fibrinogen concentration. After adding thrombin, the clotting time is recorded and compared to a calibration curve derived from samples with known fibrinogen levels.
Performing the Clauss Test
- Calibration Curve: A reference plasma (e.g., STA® Unicalibrator) with known fibrinogen concentrations is used to create a curve. Example data:
| Time (sec) | Fibrinogen (mg/dL) | Dilution |
| 10 | 608 | 1:5 |
| 18 | 304 | 1:10 |
| 25 | 204 | 1:15 |
| 32 | 152 | 1:20 |
| 44.8 | 100 | 1:30 |
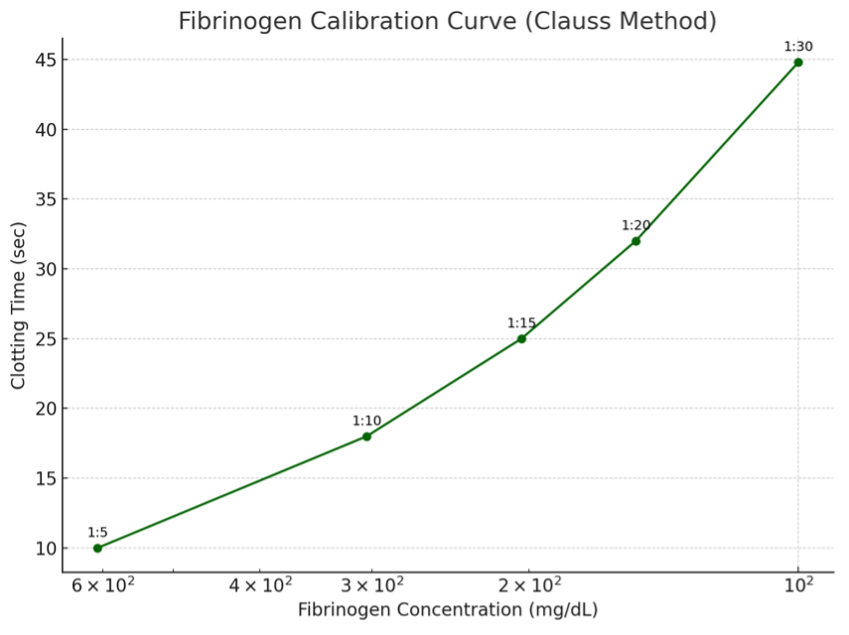
- This graph shows the relationship between clot formation time and fibrinogen concentration in the Clauss test. Each point is labeled with its corresponding dilution ratio (e.g. 1:10 or 1:30) and as you can see, the clotting time increases as the fibrinogen concentration decreases. This calibration curve is used as a reference to estimate the fibrinogen concentration in patient samples.
- Manual Method:
- Dilute the sample 1:10 with imidazole buffer (100 µL plasma + 900 µL buffer).
- Use clean glass tubes.
- Incubate 200 µL of diluted sample at 36–38°C for 2–3 minutes.
- Add 100 µL thrombin, start the timer, and record clotting time.
- Calculate fibrinogen concentration using the calibration curve.
- Semi-Automated Method:
- Dilute sample 1:10.
- Incubate 100 µL at 37°C.
- Add 50 µL thrombin and note the time.
- Derive results from the calibration curve.
Adjustments may be needed for extreme values (e.g., retesting with 1:30 or 1:3 dilutions) to ensure accuracy, avoiding interference from contaminants.
🔹 Reference Ranges and Result Interpretation
🔸 Normal Fibrinogen Ranges
- Adults: 200–400 mg/dL (indicates normal function).
- Newborns: 125–300 mg/dL (naturally lower, rising with development).
- Pregnancy: Up to 600–700 mg/dL (a physiologic increase due to hormonal changes).
🔸 Clinical Interpretation
- Below 100 mg/dL: Suggests severe bleeding, DIC, or advanced liver disease, requiring urgent attention.
- 100–200 mg/dL: Mild reduction, possibly due to minor disorders or temporary factors like inflammation—needs further investigation.
- Above 400 mg/dL: Indicates acute inflammation, cancer, or heightened cardiovascular risk, warranting additional tests.
🔹 Fibrinogen Activity vs. Antigen Levels
| Condition | Antigen Level | Activity Level | Interpretation |
| Normal | Normal | Normal | Healthy |
| Dysfibrinogenemia | Normal | Low | Structural defect, poor function |
| Hypofibrinogenemia | Low | Low | Deficiency in amount and function |
| Hyperfibrinogenemia | High | Normal | Inflammation or pregnancy |
🔹 Common Errors and Interferences
Factors like heparin in the sample can falsely lower fibrinogen results by inhibiting thrombin. High levels of fibrin degradation products (FDPs) or D-dimer can also interfere, prolonging clotting time. Temperature control (ideally 37°C) is critical, as deviations affect enzymatic reactions and skew results.
🔹 Quality Control and Validation
Regular use of normal and abnormal control samples ensures accuracy. Results must fall within manufacturer-specified ranges; deviations require troubleshooting (e.g., reagent quality, equipment function). External quality assurance programs (EQA) further validate lab performance.
🔹 Advanced Tips for Lab Experts
- Combine fibrinogen testing with PT, aPTT, and D-dimer for a fuller picture in complex cases like DIC.
- In suspected dysfibrinogenemia, compare Clauss (activity) and ELISA (antigen) results—a low activity-to-antigen ratio is diagnostic.
- For patients on heparin, use neutralizers (e.g., heparinase) to ensure accurate readings.
- In emergencies, viscoelastic devices (TEG/ROTEM) offer real-time clotting insights for rapid decision-making.
Frequently Asked Questions (FAQ)
- What is a fibrinogen test?
It measures fibrinogen levels in the blood, a protein essential for clotting and preventing excessive bleeding, aiding in diagnosing clotting disorders. - When is it needed?
It’s used for unexplained bleeding, clotting issues, liver disease, DIC, or thrombosis cases. - What do abnormal results mean?
Low levels may indicate bleeding risks (e.g., DIC, liver disease); high levels suggest inflammation or clotting risks (e.g., cardiovascular disease). - How are results interpreted?
Normal is 200–400 mg/dL. Values outside this range signal potential health issues, interpreted with clinical context. - Which conditions benefit from this test?
It helps diagnose DIC, liver disorders, inflammation, and cardiovascular risks, plus monitors clotting tendencies. - Does fibrinogen change during pregnancy?
Yes, it naturally rises (up to 600–700 mg/dL) due to hormonal shifts and increased clotting needs. - Is preparation required?
Typically, no fasting is needed, but consult your doctor, as some medications may affect results. - Is the test accurate?
Generally, yes, though inflammation, infections, or drugs can influence outcomes—medical review is key. - What affects fibrinogen levels?
Liver issues, infections, heart disease, cancer, smoking, or intense exercise can alter levels. - How can levels be improved?
It depends on the cause—treating liver disease or inflammation can help normalize levels.

